by Allison Summerton
This is the third blog in a series about shopping for health insurance in 2014. We know that cost and provider are two of the biggest factors consumers consider when looking at insurance. The first blog discussed how deductibles, copayments and coinsurance factor into the total cost of health care and the second blog discussed how different provider networks may influence your insurance plan selection.
For many, the cost of prescription drugs is also a key consideration. With this blog, we will provide some tools for looking at those costs when doing your shopping.
The Affordable Care Act requires that all plans sold on the state marketplaces provide a comprehensive set of health services, called essential health benefits, which include prescription drugs. Nationally, average out-of-pocket costs for prescription medicines for people with private insurance under age 65 were $1,146 in 2012.
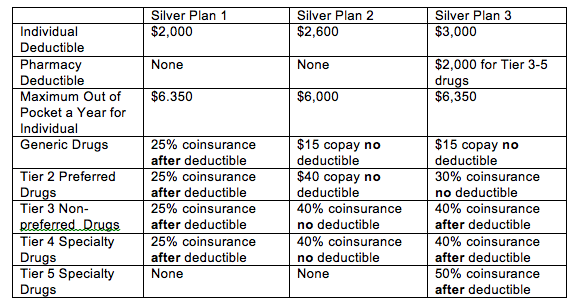
Insurance plans sold on the Connect for Health Colorado marketplace group prescription drugs into cost levels known as “tiers”. Most plans have four tiers (a few have five tiers), each with a different payment structure. The tiers are a method to hold down costs by transferring more costs to consumers for higher priced drugs.
Tier 1 contains generic drugs which are no longer covered by patent protection, are usually manufactured by multiple drug companies and are less expensive than Brand-name drugs. Most Silver, Gold and Platinum plans charge a copayment for Tier 1 drugs, typically in the $5 to $25 range.(For example $15 for a month’s supply of the generic drug.)
Tier 2 contains drugs which are on the preferred drug list and do not have a generic substitute. Preferred drugs are usually drugs the insurer has negotiated at a reduced price. Many Bronze plans require coinsurance for Tier 2, 3 and 4 drugs. (For example if the drug costs $120 a month and the coinsurance amount is 30%, you would pay $40.)
Tier 3 contains non-preferred drugs which are often brand-name drugs that have a generic substitute.
Tier 4 drugs are specialty drugs used to treat rare conditions, They usually require clinical expertise by the pharmacy for administering the drug and educating the patient. They are the most expensive drugs.
Each insurance plan has a unique list of prescription drugs they cover. This list, called a “formulary”, includes the tier for each medication. Because formularies and cost sharing policies — for example, some have a deductible for prescription drugs, others do not – vary by insurance plan, consumers who regularly take a prescription medicine should look at both components when shopping for coverage.
To give an example of the variability, here is the prescription drug coverage of three Silver plans in the Marketplace.
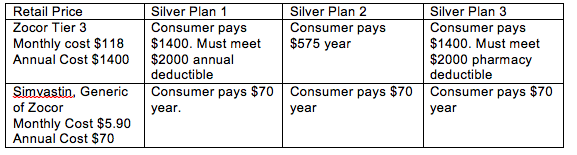
The cost impacts of these three state-wide silver plans can be dramatic.
For illustrative purposes only, let’s assume a consumer, Sam, takes a cholesterol-lowering drug Zocor, a brand-name drug that is also available in a generic form. It would be treated as a non-preferred, Tier 3 drug. The retail price at Costco is $118 for a one-month prescription, or about $1400 a year. (Note: Health plans may offer lower, negotiated drug prices.) Under plans 1 and 3, the insurer does not pay for the medicines until Sam reaches the $2,000 deductible so Sam pays the full $1,400 for the year.
However, If Sam and his health care provider decided he could get the same health benefits from the generic form of Zocor (simvastin), he would pay the lower cost of the generic drug and would be able to reduce his medication cost to $70 a year.
In addition to comparing the deductibles, copayments and co-insurance amounts for the plans, check the plan formularies to be sure it covers your medication and its cost tier. There is a link to the plan formularies on the Connect For Health Colorado website under each plan listed. If in doubt, call the health plan to confirm the coverage and cost sharing of your medication.
One final note, Obamacare requires plans to provide preventive health services to consumers without cost sharing requirements. This requirement applies to some medications such as prenatal vitamins, pediatric vitamins and birth control for women.
