By Amber Burkhart, Health Policy Fellow
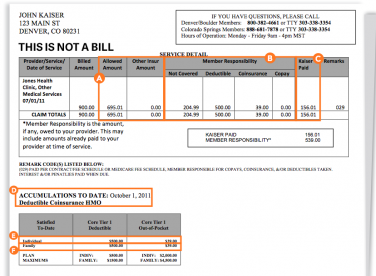
Ensuring greater transparency in the health care system is a priority for health care advocates as it enables consumers to better navigate their health insurance. What happens, however, when transparency has the unintended consequence of creating a barrier to accessing health services? Sending Explanation of Benefits (EOB) letters, which is intended to notify policyholders with a summary of services provided, may actually impede access to care for minors who are reluctant to share sensitive health concerns with their parents or guardians.
The Society of Adolescent Health found that in a national survey, 35 percent of middle and high school students that did not seek health care because they did not want their parents to find out. Examples of these situations include, but are certainly not limited to, individuals receiving care for HIV or AIDS, reproductive and sexual health care services, mental health care and substance abuse services, sexual violence and domestic/dating violence screening and services as well as services relating to an individual’s sexual orientation or gender identity.
Protections for minors’ privacy are vital to their health and safety
Undiagnosed mental health conditions, unintended pregnancy, and untreated Sexually Transmitted Infections (STIs) have serious consequences that can occur if care is delayed or forgone out of fear that a parent would have access to the EOB. For example, access to confidential mental health care services is critical during adolescents’ physical, emotional, and social development. According to the National Institute of Mental Health, 50 percent of mental health conditions occur by age 14, and 75 percent by age 24. In addition, the Colorado Department of Public Health, Office of Suicide Prevention found that suicide is the leading cause of death among Coloradans ages 10-35 and the highest rate of suicide attempts is among girls ages 12-18. Sending an EOB to a minors’ parent creates a significant barrier for that individual to confidentially access mental health services when they need them most.
Colorado Protections for Minors’ Confidentiality and New Strategies to Explore
Protections for minors’ privacy in receiving health care currently exist in Colorado law, which is an important first step. Minors may consent and confidentially access family planning services, STI/HIV diagnosis and treatment, mental health services and addiction treatments. These protections may be undermined however, if their insurance company sends a notice to the parents of the minor who sought care. Other states have implemented, or are considering, protections that Colorado could explore to provide important privacy protections to minors, including the following:
- Not requiring health plans to send an EOB when there is no balance due for services provided (implemented in New York, Wisconsin and Massachusetts).
- Applying a generic procedural terminology code to sensitive services (implemented in Erie County, New York and Massachusetts).
- Requiring plans to honor requests for confidential communications from all individuals obtaining sensitive services so that EOBs go directly to the individual seeking care or wherever they request the EOB to be sent (California SB 138 took effect January 1, 2015 and Maryland SB 790 passed in April 2014).
Transparency is important, but only when it is meaningful. We hope that Colorado will consider strategies implemented by other states and adopt regulations to protect against patient confidentiality breaches for minors seeking sensitive services. Eliminating this barrier to health care services will ensure minors receive the care they need, when they need it!
For a full review of protections states are considering or implementing read: Protecting Adolescent Confidentiality Under Health Care Reform: The Special Case Regarding Explanation of Benefits (EOBs) and Confidentiality for Individuals Insured as Dependents: A Review of State Laws and Policies.)
